Pancreatic Cancer Explained: Everything You Need to Know About This Silent Disease
Introduction
Pancreatic cancer is often called the “silent killer” because it develops with few or no symptoms in its early stages and is often diagnosed late. It is one of the deadliest cancers, with a low survival rate due to its aggressive nature and late detection. Understanding pancreatic cancer, its risk factors, symptoms, diagnosis, and treatment options, is crucial in improving awareness and early detection.
In this blog, we will discuss everything you need to know about pancreatic cancer, including its causes, symptoms, risk factors, and the latest advancements in treatment.
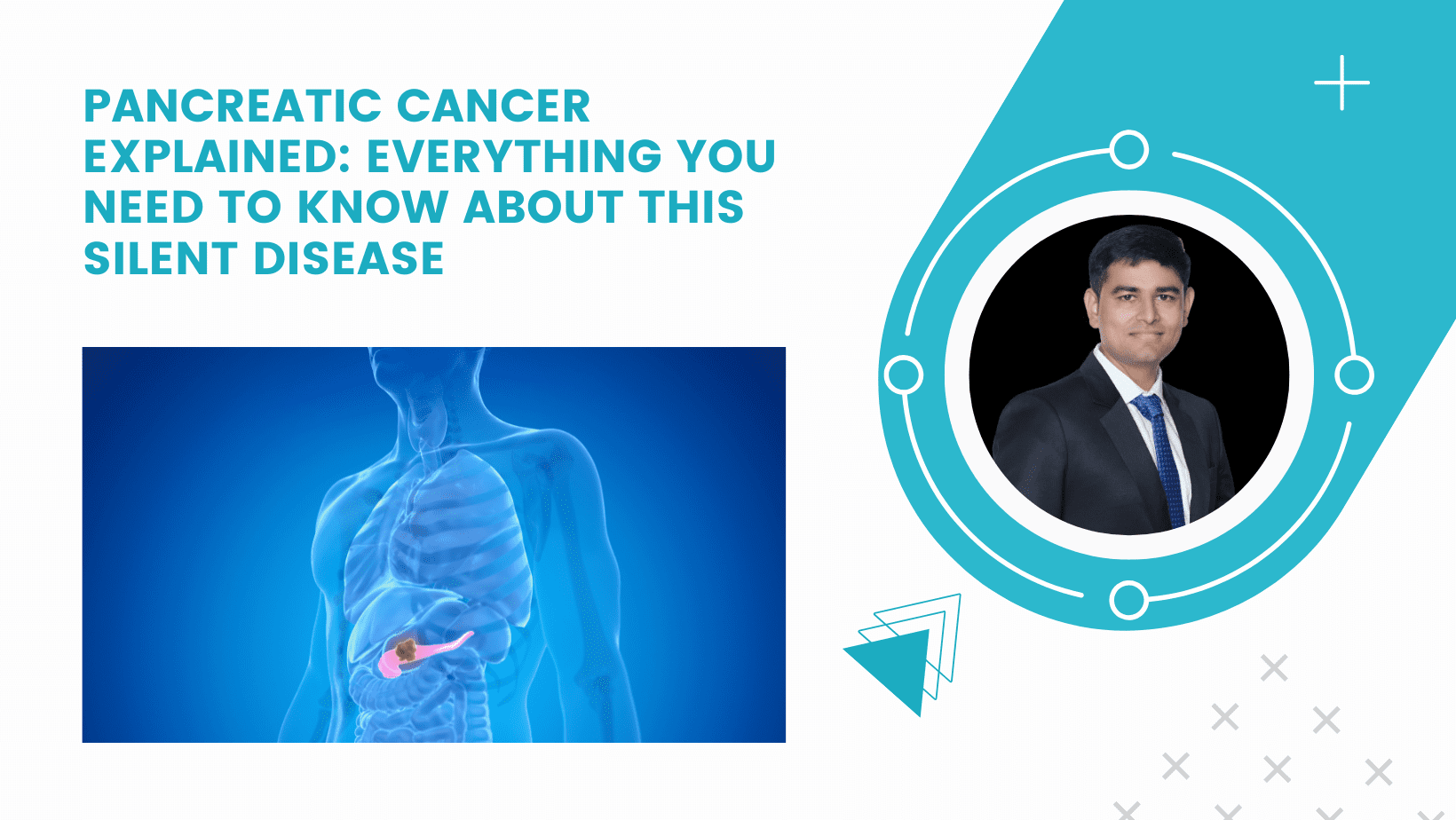
What is Pancreatic Cancer?
Pancreatic cancer begins in the tissues of the pancreas, an organ located behind the stomach that plays a key role in digestion and blood sugar regulation. The pancreas has two main functions:
- Exocrine function: Producing enzymes to help digest food.
- Endocrine function: Producing insulin and other hormones that regulate blood sugar.
Most pancreatic cancers (about 90%) are pancreatic ductal adenocarcinomas (PDAC), which arise in the exocrine cells of the pancreas. Less common types include neuroendocrine tumors (NETs), which develop in hormone-producing cells.

Why is Pancreatic Cancer Called a “Silent Disease”?
Pancreatic cancer is known as a “silent disease” because:
✅ It develops slowly and without noticeable symptoms in its early stages.
✅ The pancreas is deep inside the abdomen, making tumors difficult to detect during routine check-ups.
✅ Symptoms, when they appear, often resemble other digestive issues, leading to delayed diagnosis.
Symptoms of Pancreatic Cancer
In its early stages, pancreatic cancer rarely causes symptoms. However, as the tumor grows, patients may experience:
Early Symptoms (Often Overlooked):
🔹 Unexplained weight loss – A sudden, significant drop in weight without changes in diet or exercise.
🔹 Loss of appetite – Persistent nausea or lack of hunger.
🔹 Abdominal pain or discomfort – Pain in the upper abdomen or back, often worsening after eating.
🔹 Fatigue and weakness – Feeling constantly tired or drained.
Advanced Symptoms:
🔹 Jaundice (Yellowing of Skin & Eyes) – A sign of bile duct blockage due to tumor growth.
🔹 Dark urine and pale stools – Caused by poor bile flow from the pancreas.
🔹 New-onset diabetes – Sudden development of diabetes, especially without obesity or family history.
🔹 Digestive problems – Bloating, gas, diarrhea, and greasy stools due to improper digestion.
If you experience persistent symptoms, consult a gastroenterologist or specialist immediately for further evaluation.
Risk Factors for Pancreatic Cancer
Several factors increase the risk of developing pancreatic cancer:
Non-Modifiable Risk Factors (Cannot be Changed):
🔹 Age – Most cases occur in people above 60 years old.
🔹 Family history – Having a close relative with pancreatic cancer increases risk.
🔹 Genetic mutations – BRCA1, BRCA2, and Lynch syndrome genes are linked to pancreatic cancer.
Modifiable Risk Factors (Can be Controlled):
🔹 Smoking – Doubles the risk of developing pancreatic cancer.
🔹 Obesity – Being overweight is linked to higher insulin levels, which may promote tumor growth.
🔹 Chronic pancreatitis – Long-term inflammation of the pancreas increases cancer risk.
🔹 Diabetes – Type 2 diabetes is associated with a higher risk of pancreatic cancer.
🔹 Heavy alcohol consumption – Excessive drinking may lead to chronic pancreatitis, a known risk factor.
Preventive Measures:
✅ Quit smoking – Reduces risk significantly.
✅ Maintain a healthy diet – Eat fruits, vegetables, whole grains, and lean proteins while avoiding processed foods.
✅ Exercise regularly – Helps regulate blood sugar and reduces obesity-related risks.
✅ Limit alcohol consumption – Protects against pancreatitis and other digestive disorders.

How is Pancreatic Cancer Diagnosed?
Because early symptoms are vague, pancreatic cancer is often detected in later stages. Doctors use various tests to confirm the diagnosis:
1. Imaging Tests:
🔹 CT Scan & MRI – Provides detailed images of the pancreas and surrounding tissues.
🔹 Endoscopic Ultrasound (EUS) – A small camera inserted through the mouth to examine the pancreas.
🔹 PET Scan – Identifies cancerous cells throughout the body.
2. Blood Tests:
🔹 CA 19-9 Test – A tumor marker test used to monitor treatment response but not for early detection.
3. Biopsy:
🔹 A sample of pancreatic tissue is taken and analyzed under a microscope to confirm cancer.
Treatment Options for Pancreatic Cancer
Treatment depends on the stage of cancer, overall health, and tumor location.
1. Surgery (For Early-Stage Cancer):
- Whipple Procedure (Pancreaticoduodenectomy): Removes part of the pancreas, bile duct, and small intestine.
- Distal Pancreatectomy: Removes the tail and part of the body of the pancreas.
- Total Pancreatectomy: Removes the entire pancreas (rarely performed).
2. Chemotherapy:
Used to shrink tumors before surgery or slow the cancer’s progression in advanced stages.
3. Radiation Therapy:
High-energy beams target and destroy cancer cells. Often used with chemotherapy.
4. Immunotherapy & Targeted Therapy (For Advanced Cases):
New treatments that boost the immune system or specifically target cancerous cells.
5. Palliative Care (For Late-Stage Cancer):
Focuses on pain management, improving quality of life, and symptom control in advanced cases.
Survival Rate & Outlook
Pancreatic cancer has a low survival rate, but early detection improves outcomes.
- Localized cancer (early stage): 5-year survival rate is ~44%.
- Regionally spread cancer: Survival rate drops to ~15%.
- Metastatic cancer (advanced stage): Survival rate is ~3%.
Early detection and advancements in treatment are key to improving survival rates.
Conclusion: Raising Awareness & Seeking Timely Medical Help
Pancreatic cancer is a serious but often overlooked disease due to its silent symptoms and late detection. Regular health check-ups, awareness of symptoms, and a healthy lifestyle can help reduce the risk and improve early diagnosis.
If you or someone you know experiences persistent digestive issues, unexplained weight loss, or jaundice, consult a gastroenterologist immediately. Early intervention can save lives.
🔹 Have questions about pancreatic health? Contact Dr.Gastro.in for expert consultation and guidance.







Leave a Reply