Gall Bladder Stone Treatment in Ahmedabad: Latest Options & Recovery Tips
Gall bladder stones—commonly known as gallstones—are a widespread digestive issue that can cause sudden pain and serious complications. If you are searching for Gall Bladder Stone Treatment in Ahmedabad, understanding the causes, modern treatment options and the recovery process is the first step toward permanent relief. This comprehensive guide explains everything you need to know, from early symptoms to advanced medical care.
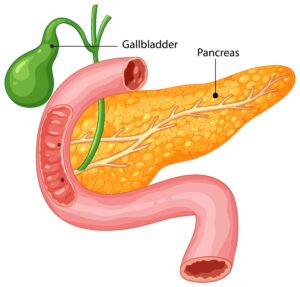
What Are Gall Bladder Stones?
The gall bladder is a small, pear-shaped organ located beneath the liver. Its main function is to store and release bile, a fluid that helps digest fats. When bile contains too much cholesterol, bilirubin or certain salts, it can crystallise and form hard deposits called gallstones. These stones can be as tiny as a grain of sand or as large as a golf ball.

Key Symptoms to Watch For
-
Sudden, sharp pain in the upper right abdomen or centre of the stomach (known as biliary colic)
-
Nausea or vomiting, especially after heavy meals
-
Indigestion, bloating and discomfort when consuming fatty foods
-
Fever, chills or jaundice if infection or bile duct blockage occurs
Not everyone with gallstones experiences symptoms, but when pain or digestive trouble begins, professional evaluation is critical.
Diagnosis: How Doctors Confirm the Condition
Specialists offering Gall Bladder Stone Treatment in Ahmedabad use a combination of tests to confirm the presence of stones and determine the right approach:
-
Abdominal Ultrasound – The most common, painless imaging test to detect gallstones and inflammation.
-
CT Scan or MRI – Used when complications or more detailed images are needed.
-
Blood Tests – To check for infection, liver enzyme abnormalities and pancreatic involvement.
Prompt diagnosis ensures you receive treatment before complications such as infection, pancreatitis or bile duct obstruction develop.
Latest Treatment Options
Modern medicine provides both surgical and non-surgical methods for Gall Bladder Stone Treatment in Ahmedabad. The right choice depends on the size of the stones, the severity of symptoms and overall health.
1. Laparoscopic Cholecystectomy
This minimally invasive surgery is the gold standard for most patients. Through 3–4 tiny incisions, the surgeon removes the gall bladder entirely, preventing future stone formation.
Benefits include:
-
Very small scars and minimal post-operative pain
-
Short hospital stay, often just 24–48 hours
-
Quick return to routine activities—usually within a week
Because the gall bladder’s function is not essential for normal digestion, removing it has little long-term impact.
2. Endoscopic or ERCP Procedures
If a gallstone has migrated into the bile duct, doctors may perform an endoscopic procedure called ERCP (Endoscopic Retrograde Cholangiopancreatography) to remove the stone without a large incision.
3. Non-Surgical Management
For patients who cannot undergo surgery or who have small cholesterol stones, medications such as ursodeoxycholic acid can slowly dissolve stones. However, this method is less common because it may take months and stones can recur.
4. Lifestyle and Dietary Adjustments
While not a cure once stones have formed, dietary changes—such as reducing saturated fat, maintaining a healthy weight and increasing fibre intake—can prevent further gallstone development and support recovery after treatment.
Preparing for Gall Bladder Stone Surgery
If your gastroenterologist recommends laparoscopic cholecystectomy, preparation is straightforward:
-
Medical evaluation: Blood tests, imaging and anaesthetic assessment
-
Medication review: Your doctor will advise if you need to stop blood thinners or adjust any regular medicines
-
Pre-operative fasting: Typically no food or drink for at least six hours before surgery
Clear communication with your surgeon ensures a smooth experience and reduces anxiety.
Recovery Tips After Treatment
Patients undergoing Gall Bladder Stone Treatment in Ahmedabad can expect a fast and comfortable recovery if they follow medical advice:
-
Follow a low-fat diet initially: Start with light, easily digestible meals for the first week.
-
Stay hydrated: Adequate fluid intake helps your body heal and maintain good digestion.
-
Gentle movement: Light walking improves circulation and prevents post-operative complications.
-
Wound care: Keep the incision area clean and dry, and follow your doctor’s instructions for dressing changes.
-
Regular follow-ups: Attend all scheduled appointments to monitor healing and address any concerns promptly.
Most people return to work or normal activities within 7–10 days after laparoscopic surgery. Heavy lifting should be avoided for at least four weeks.
Why Choose Ahmedabad for Gall Bladder Stone Treatment
Ahmedabad is home to advanced gastroenterology centres and highly skilled surgeons who specialise in minimally invasive procedures. Choosing a local specialist means:
-
Cutting-edge facilities: Hospitals equipped with state-of-the-art laparoscopic and endoscopic technology.
-
Experienced surgeons: Doctors with extensive expertise in treating complex gall bladder conditions.
-
Comprehensive aftercare: From diagnosis to follow-up, patients receive personalised support for a smooth recovery.
Preventing Future Gallstone Problems
Even after gall bladder removal, maintaining healthy habits can support overall digestive health:
-
Maintain a balanced diet rich in fruits, vegetables and lean proteins.
-
Exercise regularly to keep body weight stable.
-
Stay hydrated and avoid crash diets or sudden weight loss, which can increase bile cholesterol levels.
These simple lifestyle steps promote long-term digestive wellness and reduce the risk of other gastrointestinal issues.
When to Seek Immediate Medical Help
Seek urgent care if you experience:
-
Intense abdominal pain that lasts more than a few hours
-
High fever or chills
-
Yellowing of the skin or eyes (jaundice)
-
Persistent vomiting
These may signal complications such as infection or pancreatitis and require emergency treatment.
The Bottom Line
Gall bladder stones can be painful and disruptive, but timely diagnosis and modern medical care provide lasting relief. With advanced laparoscopic surgery and expert gastroenterologists available locally, Gall Bladder Stone Treatment in Ahmedabad is both safe and highly effective.
If you’re experiencing symptoms or have been diagnosed with gallstones, don’t delay. Schedule a consultation today through drgastro.in to discuss the best treatment option and start your journey toward a healthier, pain-free life.