Can You Reverse Fatty Liver? A Guide to Managing MASLD
If you have recently had an ultrasound or blood work done, you might have heard your doctor say something like: "Everything looks fine, but you have a little bit of fatty liver. Try to eat better."
You are not alone. It is estimated that 1 in 4 adults worldwide has excess fat in their liver. It is the most common chronic liver disease on the planet.
For years, this condition was brushed off as a minor issue. But in the medical community, the alarm bells are ringing. We now know that fatty liver is not just a benign condition—it is a "silent epidemic" that can lead to severe scarring (cirrhosis), liver failure, and even cancer if left unchecked.
The good news? The liver is the only organ in your body that can regenerate. Unlike heart disease or kidney damage, fatty liver is often 100% reversible if caught early.
In this guide, we will break down the new name for the disease (MASLD), the silent symptoms you might be missing, and the exact roadmap to healing your liver.


First: Why Is the Name Changing? (NAFLD vs. MASLD)
If you are researching online, you will see two acronyms: NAFLD and MASLD. They refer to the same condition, but the medical world is undergoing a major re-branding.- The Old Name: Non-Alcoholic Fatty Liver Disease (NAFLD).
- The Problem: This defined the disease by what it wasn't (alcohol-related). It was confusing and stigmatizing.
- The New Name: Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD).
- The Benefit: This name tells us the cause. It links liver health directly to your metabolism—specifically how your body handles sugar, insulin, and weight.

What Is Happening Inside Your Liver?
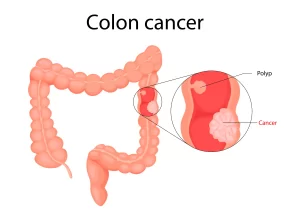
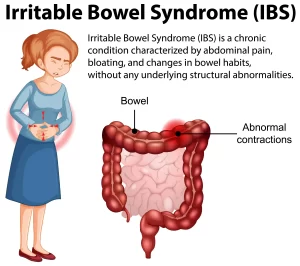
Your liver is the body's filter and chemical factory. It processes everything you eat and drink. A healthy liver should contain little to no fat. When you consume more calories—specifically from sugars and refined carbohydrates—than your body can burn, the liver turns that excess energy into fat molecules (triglycerides). These fat cells infiltrate the liver tissue. Think of it like a sponge soaked in grease.- Steatosis (Simple Fatty Liver): There is fat, but no inflammation. The liver is working, but it’s under stress.
- MASH (Metabolic Dysfunction-Associated Steatohepatitis): The fat is now causing inflammation. The liver cells are swelling and dying. This is the danger zone.
- Fibrosis/Cirrhosis: The liver tries to heal the inflammation by creating scar tissue. Eventually, the liver becomes hard and lumpy (cirrhosis), leading to permanent failure.
The "Silent" Symptoms: How to Know If You Have It
The scariest part of MASLD is that it is usually asymptomatic until the damage is advanced. You cannot "feel" your liver getting fatter. However, many patients report subtle signs that they often attribute to aging or stress:- Chronic Fatigue: A deep tiredness that sleep doesn't fix. The liver regulates energy storage; when it’s struggling, your energy crashes.
- Right Upper Quadrant Discomfort: A dull ache or feeling of "fullness" under your right rib cage. This isn't usually sharp pain; it’s the sensation of the liver physically enlarging and pressing on its capsule.
- Brain Fog: Difficulty concentrating or feeling "fuzzy."
- Signs of Insulin Resistance: Dark patches of skin on the neck or armpits (Acanthosis Nigricans) or skin tags.
Diagnosis: Beyond the Blood Test
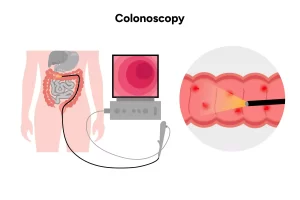
"But my blood work was normal!" We hear this often. Standard liver enzymes (AST and ALT) can be completely normal even in patients with significant fatty liver. You cannot rely on basic blood work alone. To get a true picture, Gastroenterologists use:- Ultrasound: Good for seeing if fat is present.
- FibroScan (Transient Elastography): This is a game-changer. It is a specialized ultrasound that measures the stiffness of your liver. It tells us specifically if you have scarring (Fibrosis) without needing a painful needle biopsy.
The Cure: How to Reverse It (No Pills Required)
Currently, there are very few FDA-approved medications specifically for fatty liver (though some new diabetes drugs are showing promise). The primary treatment—and the only one that works for almost everyone—is Lifestyle Medicine.1. The 10% Weight Loss Rule
You do not need to become a supermodel to fix your liver. Studies show that losing just 7% to 10% of your body weight is enough to:- Remove the fat from the liver.
- Reverse inflammation.
- Even reverse early scarring (fibrosis). For a 200lb person, that is just 20lbs. It is a clearly defined, achievable target.
2. The Enemy is Sugar, Not Fat
For decades, people thought "eating fat makes a fatty liver." We now know the bigger culprit is Fructose (sugar). High Fructose Corn Syrup and refined white sugar hit the liver like a bomb, triggering immediate fat production.- The Fix: Eliminate sugary sodas, juices, and limit added sugars. Your liver will thank you within days.
3. The Mediterranean Diet Approach
This is the most evidence-based diet for liver health.- Eat: Olive oil, avocados, nuts (Healthy Fats), fatty fish (Omega-3s), and loads of vegetables.
- Avoid: Processed meats, white bread, and boxed snacks.
4. The "Coffee" Prescription
This is the one piece of advice patients love. Multiple large-scale studies have shown that drinking coffee is protective for the liver. It lowers liver enzymes and reduces the risk of scarring.- The Dose: 2 to 3 cups of black coffee (caffeinated or decaf) per day seems to be the sweet spot. Just don't load it with sugar!
"Lean" Fatty Liver: It’s Not Just About Weight
It is crucial to note that "skinny" people can get this too. This is called Lean MASLD. Genetics, poor diet (high sugar/processed food), and visceral fat (fat hidden around the organs) can cause fatty liver in people with a normal BMI. If you are thin but have high cholesterol, pre-diabetes, or a family history, you should still be screened.
When to See a Specialist
If you have been diagnosed with fatty liver, don't ignore it. You need to know where you stand on the spectrum.- Do you have simple fat? Or do you have scarring (fibrosis)?