Expert Solutions for Non-Alcoholic Fatty Liver Disease (NAFLD) in Science City, Sola Ahmedabad
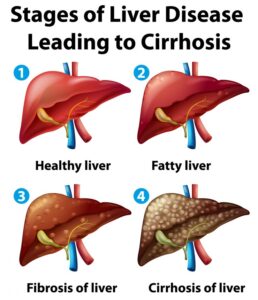
Non-Alcoholic Fatty Liver Disease (NAFLD) is a growing health concern worldwide, and its prevalence in urban areas like Science City, Sola, Ahmedabad, is increasing. Characterized by the accumulation of excess fat in the liver, NAFLD can lead to severe complications, including liver inflammation, fibrosis, or even cirrhosis if left untreated. Fortunately, expert care and innovative treatment options are readily available in Science City, Sola, Ahmedabad, ensuring better outcomes for patients.


What is NAFLD?
NAFLD refers to a spectrum of liver conditions unrelated to alcohol consumption. It primarily occurs due to metabolic conditions such as obesity, type 2 diabetes, high cholesterol, or a sedentary lifestyle. NAFLD is often referred to as a silent disease because most individuals show no symptoms until it has progressed significantly.Symptoms to Watch Out For
While many individuals with NAFLD are asymptomatic, some may experience:- Fatigue
- Abdominal pain or discomfort, especially in the upper right quadrant
- Unexplained weight loss
- Weakness or a general feeling of being unwell
Expert Care for NAFLD in Science City, Sola Ahmedabad
In Science City, Sola, Ahmedabad, medical practitioners and hospitals are equipped with advanced tools and technologies to address NAFLD effectively. Here's how expert solutions can help:1. Comprehensive Diagnosis
NAFLD diagnosis involves:- Blood Tests: Liver function tests to detect abnormalities.
- Ultrasound or Fibroscan: Imaging studies to evaluate fat accumulation in the liver.
- Biopsy: In some cases, a liver biopsy is performed to confirm the severity of the disease.
2. Lifestyle Interventions
Expert doctors emphasize the importance of lifestyle changes in managing NAFLD. These include:- Healthy Diet: A balanced diet rich in whole grains, lean proteins, healthy fats, and vegetables can reverse fat buildup in the liver.
- Regular Exercise: Engaging in moderate-intensity aerobic exercises for at least 30 minutes a day.
- Weight Loss: Losing 5–10% of body weight can significantly improve liver health.
3. Medical Management
For advanced cases of NAFLD, medical experts in Science City, Sola, Ahmedabad, may recommend:- Medications: To manage underlying conditions like insulin resistance, high cholesterol, or liver inflammation.
- Antioxidants and Supplements: Vitamin E and other supplements to reduce oxidative stress in the liver.
- Monitoring of Comorbidities: Controlling conditions like diabetes and hypertension is crucial to preventing NAFLD progression.
4. Advanced Treatment Options
In severe cases, specialized procedures and surgical interventions may be necessary. This includes:- Liver Transplant: For end-stage liver disease or cirrhosis.
- Endoscopic Procedures: To manage complications and improve liver function.
Why Choose Science City, Sola Ahmedabad for NAFLD Treatment?
Science City, Sola, Ahmedabad, is home to renowned hospitals and healthcare professionals specializing in gastroenterology. The region offers:- Expert Gastroenterologists: Skilled professionals with years of experience in diagnosing and managing NAFLD.
- Cutting-Edge Facilities: Access to advanced diagnostic tools like Fibroscan and non-invasive imaging techniques.
- Holistic Care: Customized treatment plans that focus on both physical and mental well-being.
Preventing NAFLD: Tips from Experts in Science City, Sola Ahmedabad
- Adopt a Balanced Diet: Limit sugar and saturated fat intake while increasing fiber consumption.
- Stay Active: Incorporate daily physical activity into your routine.
- Regular Health Checkups: Schedule routine liver health screenings, especially if you are at risk of developing NAFLD.
- Avoid Unnecessary Medications: Over-the-counter drugs, when taken excessively, can harm the liver.



 Dr. Patel’s Approach to Gall Bladder Surgery
Dr. Patel is known for his thorough, patient-focused approach. From diagnosis through recovery, he prioritizes clear communication and compassionate care. Patients receive all necessary information to feel prepared for their procedure and are supported with post-operative care that promotes fast healing and a smooth return to daily activities.
Choosing Dr. Hamikchandra Patel for gall bladder surgery means opting for expertise and compassion. If you’re in Sola, Ahmedabad, and dealing with gall bladder issues, schedule a consultation with Dr. Patel to discuss your treatment options.
Dr. Patel’s Approach to Gall Bladder Surgery
Dr. Patel is known for his thorough, patient-focused approach. From diagnosis through recovery, he prioritizes clear communication and compassionate care. Patients receive all necessary information to feel prepared for their procedure and are supported with post-operative care that promotes fast healing and a smooth return to daily activities.
Choosing Dr. Hamikchandra Patel for gall bladder surgery means opting for expertise and compassion. If you’re in Sola, Ahmedabad, and dealing with gall bladder issues, schedule a consultation with Dr. Patel to discuss your treatment options.
 Why Patients Trust Dr. Patel for Fistula Surgery
Dr. Patel is committed to patient comfort and positive outcomes. He provides detailed guidance on each step of the treatment process, explaining the benefits of different procedures and setting clear expectations. Patients appreciate his clear communication and compassionate approach, which make a challenging experience easier to manage.
For those suffering from fistulas in Sola, Ahmedabad, Dr. Patel’s expertise in minimally invasive fistula surgery offers a path to effective treatment and long-term relief. Schedule a consultation with Dr. Patel to learn more about your options.
Why Patients Trust Dr. Patel for Fistula Surgery
Dr. Patel is committed to patient comfort and positive outcomes. He provides detailed guidance on each step of the treatment process, explaining the benefits of different procedures and setting clear expectations. Patients appreciate his clear communication and compassionate approach, which make a challenging experience easier to manage.
For those suffering from fistulas in Sola, Ahmedabad, Dr. Patel’s expertise in minimally invasive fistula surgery offers a path to effective treatment and long-term relief. Schedule a consultation with Dr. Patel to learn more about your options.
 Personalized Care for Lasting Health
Dr. Patel’s holistic approach to treatment includes not only medical interventions but also lifestyle and dietary recommendations that promote long-term health. He believes in educating his patients about their conditions, empowering them to make informed choices about their health.
Patients who work with Dr. Patel benefit from his expertise, empathy, and dedication to providing the highest level of care. For those in Sola, Ahmedabad, looking for a trusted gastroenterologist, Dr. Patel offers a pathway to better digestive health and quality of life.
Personalized Care for Lasting Health
Dr. Patel’s holistic approach to treatment includes not only medical interventions but also lifestyle and dietary recommendations that promote long-term health. He believes in educating his patients about their conditions, empowering them to make informed choices about their health.
Patients who work with Dr. Patel benefit from his expertise, empathy, and dedication to providing the highest level of care. For those in Sola, Ahmedabad, looking for a trusted gastroenterologist, Dr. Patel offers a pathway to better digestive health and quality of life.
 The Patient Experience with Dr. Patel
Patients appreciate Dr. Patel’s clear communication and empathy, which are essential when undergoing surgery. From the initial consultation to post-surgery follow-ups, Dr. Patel ensures that each patient understands their treatment plan and feels confident in their care. This dedication to patient well-being is why Dr. Patel stands out as the best choice for hernia treatment in Ahmedabad.
If you’re experiencing hernia symptoms and looking for reliable, compassionate care, schedule a consultation with Dr. Patel today to discuss how he can help you on your path to recovery.
The Patient Experience with Dr. Patel
Patients appreciate Dr. Patel’s clear communication and empathy, which are essential when undergoing surgery. From the initial consultation to post-surgery follow-ups, Dr. Patel ensures that each patient understands their treatment plan and feels confident in their care. This dedication to patient well-being is why Dr. Patel stands out as the best choice for hernia treatment in Ahmedabad.
If you’re experiencing hernia symptoms and looking for reliable, compassionate care, schedule a consultation with Dr. Patel today to discuss how he can help you on your path to recovery.
 Dr. Patel’s Approach to Hernia Surgery
Dr. Hamikchandra Patel specializes in minimally invasive hernia surgery, using laparoscopic techniques to repair the hernia with minimal incisions. This approach reduces recovery time, minimizes pain, and lowers the risk of infection. Dr. Patel also offers comprehensive pre- and post-operative care, ensuring that his patients feel supported and informed every step of the way.
For those seeking relief from hernia pain, Dr. Patel’s combination of surgical skill and compassionate care makes him one of the most trusted hernia surgeons in Sola, Ahmedabad. Book a consultation with Dr. Patel to explore your treatment options.
Dr. Patel’s Approach to Hernia Surgery
Dr. Hamikchandra Patel specializes in minimally invasive hernia surgery, using laparoscopic techniques to repair the hernia with minimal incisions. This approach reduces recovery time, minimizes pain, and lowers the risk of infection. Dr. Patel also offers comprehensive pre- and post-operative care, ensuring that his patients feel supported and informed every step of the way.
For those seeking relief from hernia pain, Dr. Patel’s combination of surgical skill and compassionate care makes him one of the most trusted hernia surgeons in Sola, Ahmedabad. Book a consultation with Dr. Patel to explore your treatment options.