Gut Health and Its Impact on Chronic Diseases Like Diabetes
In recent years, gut health has become a major focus in the medical and wellness fields, with researchers uncovering the vital role it plays in overall health. One of the most significant findings is the connection between gut health and chronic diseases, particularly diabetes. With millions of people worldwide affected by diabetes, understanding how our gut health influences this condition is critical for prevention and management. In this blog, we will explore the relationship between gut health and diabetes, and how maintaining a healthy gut may reduce the risk of developing diabetes or help in managing the condition better.


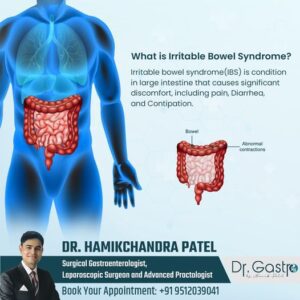
What Is Gut Health?
Gut health refers to the balance of microorganisms that live in the digestive tract. These microorganisms, often referred to as the gut microbiome, include trillions of bacteria, viruses, fungi, and other microbes that play crucial roles in digestion, immune system function, and even mental health. A healthy gut has a diverse microbiome with the right balance of good and bad bacteria. When this balance is disrupted due to poor diet, stress, or other factors, it can lead to a condition known as dysbiosis, where harmful bacteria dominate, leading to digestive issues and a host of other health problems.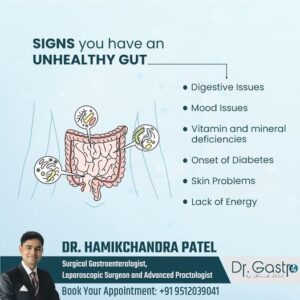
The Link Between Gut Health and Chronic Diseases
Gut health impacts more than just digestion. Research has revealed that an unhealthy gut can contribute to chronic diseases, including diabetes. Chronic inflammation, one of the key drivers of many diseases, often originates from poor gut health. When the gut lining becomes compromised (a condition sometimes called "leaky gut"), toxins and bacteria can escape into the bloodstream, triggering inflammation. This inflammation can disrupt insulin production and sensitivity, two critical factors in the development of type 2 diabetes. Moreover, the gut microbiome plays a direct role in metabolizing nutrients and regulating blood sugar levels, both of which are critical in managing or preventing diabetes.How Poor Gut Health Can Lead to Diabetes
- Impaired Blood Sugar Regulation: The gut microbiome plays a role in regulating blood sugar levels. Certain bacteria help break down fiber and produce short-chain fatty acids, which are essential for maintaining stable blood sugar. An imbalance in gut bacteria can interfere with this process, leading to blood sugar spikes and insulin resistance—a precursor to type 2 diabetes.
- Increased Inflammation: Chronic low-grade inflammation is a major factor in the development of diabetes. Poor gut health can trigger inflammation by allowing harmful substances to leak through the gut lining into the bloodstream. This condition, known as intestinal permeability or "leaky gut," can cause widespread inflammation, impairing the body’s ability to use insulin effectively.
- Obesity and Weight Gain: Obesity is one of the leading risk factors for developing type 2 diabetes. Studies show that certain types of gut bacteria can influence weight gain by affecting how the body stores fat, absorbs nutrients, and feels hungry. An unhealthy gut microbiome can disrupt these processes, leading to obesity and, eventually, diabetes.
- Metabolic Syndrome: Gut health is intricately linked to metabolic syndrome, a cluster of conditions that include high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels. These conditions increase the risk of type 2 diabetes, and an unhealthy gut can worsen them.
How to Improve Gut Health and Reduce Diabetes Risk
Fortunately, there are several ways to improve gut health, which can help reduce the risk of diabetes or manage the condition more effectively:- Eat a High-Fiber Diet: Fiber is essential for feeding beneficial gut bacteria. Foods rich in fiber, such as fruits, vegetables, legumes, and whole grains, help diversify the gut microbiome and support blood sugar regulation. Aim for 25–30 grams of fiber per day to support gut health.
- Consume Probiotic-Rich Foods: Probiotics are beneficial bacteria that can help restore balance in the gut. Fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha are rich in probiotics. These foods can help reduce inflammation, improve digestion, and enhance insulin sensitivity.
- Limit Sugar and Processed Foods: High-sugar and processed foods can feed harmful bacteria in the gut, leading to imbalances that trigger inflammation and insulin resistance. Reducing these foods in your diet can promote a healthier gut microbiome.
- Exercise Regularly: Physical activity not only helps with weight management but also positively affects gut bacteria. Regular exercise has been shown to increase the diversity of the gut microbiome, improve blood sugar control, and reduce inflammation.
- Stay Hydrated: Drinking enough water is crucial for digestion and maintaining the mucosal lining of the intestines, which supports a healthy gut environment. Staying hydrated can also aid in weight loss and improve metabolic health, reducing diabetes risk.
- Manage Stress: Chronic stress can negatively impact gut health by disrupting the balance of gut bacteria and increasing gut permeability. Practicing stress-reduction techniques such as meditation, yoga, deep breathing, and mindfulness can improve both gut and overall health.
- Consider Prebiotics: Prebiotics are compounds in food that feed the good bacteria in your gut. Foods rich in prebiotics, such as onions, garlic, asparagus, and bananas, can help maintain a healthy balance of gut bacteria.